Intracranial atheromatosis, dissection and sinus vein thrombosis
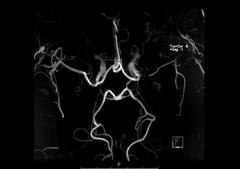
Intracranial Stenoses
Intracranial stenoses are highly prevalent and one of the main aetiologies for ischaemic stroke from a worldwide point of view. They have been shown to account for up to half of cerebrovascular ischaemic events in Asians, for up to 1/6 in Blacks and Hispanics and for up to 1/10 in Caucasians. Several pathophysiological mechanisms have been discussed in patients with intracranial stenoses resulting in symptomatic disease. Most frequent mechanisms are artery-to-artery embolism, obstruction of small penetrating arteries and impaired washout of emboli in hypoperfused cerebral tissue with/without poor collaterals. Whether there is underlying atherosclerosis or another rarer aetiology has therapeutic and prognostic implications. Advancing neuroimaging technologies facilitate determination of these pathophysiological mechanisms by improvements in spatial resolution and imaging quality of intracranial vessel lumen and morphology as well as of brain parenchyma.
In our prospective 3 years’ observational study (SAISS – Swiss Asymptomatic and Symptomatic Stenosis Study), one in three patients with a symptomatic atherosclerotic intracranial stenosis suffered a cerebrovascular event, three in five a vascular event and two in five ≥2 vascular events, despite best prevention management. We concluded, that there is an unmet need for more rigorous and effective preventive strategies in patients with symptomatic atherosclerotic intracranial stenoses (Fischer et al, J Neurol 2020).
The impact of vessel wall, luminal and parenchymal characteristics on outcome in patients with symptomatic and asymptomatic intracranial stenosis is not yet entirely clear and currently matter of research in the Bernese Intracranial Stenosis Study (BISS, PI PD Mirjam Heldner and PD Pasquale Mordasini).
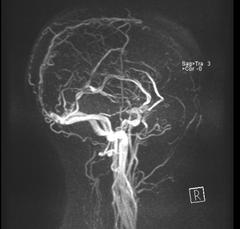
Cerebral Venous Sinus Thrombosis
Patients with cerebral venous sinus thrombosis (CVST) have an occlusion of one or more veins or dural sinuses of the brain. In a proportion of patients a venous infarct develops. In contrast to arterial stroke, CVST typically affects younger people. The diagnosis is based on clinical data, imaging and laboratory findings, but also on clinical scores (Heldner et al, Neurology 2020). Besides from focal-neurological deficits, which are the result of parenchymal injury, patients with CVST may suffer from epileptic seizures (Lindgren et al, 2020 Neurology; Sanchez van Kammen et al, Neurology 2020). Patients with CVST are currently treated with anticoagulants for at least 3 to 12 months after diagnosis, to prevent worsening of the CVST and recurrent thrombosis, and to promote venous reperfusion. The Bernese Stroke Center is contributing to the international, prospective, comparative cohort DOAC-CVST study, which assesses the safety and efficacy of direct oral anticoagulants (DOAC) compared to vitamin K antagonists for the treatment of patients with CVST (national PI PD Mirjam Heldner).
CVST became increasingly important after occurrence of severe cases in association with thrombocytopenia and anti-PF4 antibodies after SARS-Cov2 vaccination with the ChAdOx1 nCoV-19 and Ad26.COV2.S COVID-19 vaccines, mostly in young women. Recently, the ICVTC Consortium could show, that in patients with CVST prior to the COVID-19 pandemic, baseline thrombocytopenia was uncommon, and heparin-induced thrombocytopenia and anti-PF4/heparin antibodies were rare. These findings may inform investigations of the possible association between the ChAdOx1 nCoV-19 and Ad26.COV2.S COVID-19 vaccines and CVST with thrombocytopenia (Sanchez van Kammen and Heldner, JAMA 2021). Furthermore, the ICVTC Consortium underlined the findings, that CVST occurring after ChAdOx1 nCov-19 vaccination has a clinical profile, such as being associated with thrombocytopenia, distinct from CVST unrelated to vaccination (Krzywicka and Heldner, Eur J Neurol 2021).
Different clinical and research questions in relation to CVST are currently investigated by the International Cerebral Venous Thrombosis Consortium (ICVTC, https://cerebralvenousthrombosis.com), in which PD Mirjam Heldner and Prof Marcel Arnold are core members.
Secondary Stroke Prevention
The INTERSTROKE study showed that treatment of vascular risk factors greatly reduces the risk of first ever stroke. However, not all ischaemic strokes can be prevented – in Switzerland 16’000 new ischaemic strokes occur every year. Ischaemic stroke cause, besides obvious focal neurological deficits, also dementia, neurocognitive deficits, depression and fatigue. Therefore, implementing secondary prevention measures such as regular physical activity, smoking cessation and eating a healthy Mediterranean diet becomes increasingly difficult. Besides stroke-related physical and psychological limitations, stroke-survivors suffer from low self-efficacy (or self-confidence), which hamper the intrinsic motivation of implementing secondary preventive measures. In Swiss stroke survivors, it is not known to which extent the secondary prevention measures are implemented. This is subject to ongoing research at our centre (PD Mirjam Heldner and Prof Hakan Sarikaya).
One in four stroke survivors suffer a new stroke after five years, further increasing the burden of stroke. Therefore, high quality secondary preventive measures are of huge importance in preventing further cerebrovascular events. Besides prescription drugs (eg antithrombotic therapy, statins etc.), access to educative and therapy programs are needed to ensure an efficient secondary prevention. These are however expensive and not readily available. Whether the socio-economic status has an impact on the quality of secondary prevention measures is not clear and matter of ongoing investigation (SEPAIS study, PD Mirjam Heldner and Prof Marcel Arnold).
Dissection
Cervical artery dissection is a common cause of stroke in young and middle-aged adults with peak of incidence at the age of 45. The most common type is extracranial internal carotid dissection, which accounts for 2.5% of all strokes. At the dissection site formation of thrombi occur, hence it was thought that administration of anticoagulants with vitamin K antagonists (VKA) are absolutely necessary for long term secondary prophylaxis. The prospective TREAT-CAD multicentre study, with Prof Marcel Arnold as lead investigator (Engelter et al, Lancet 2021) could not show that aspirin is non-inferior to VKA. Since the trial had a non-inferiority design, a definite conclusion about the best secondary prevention after cervical artery dissection cannot be drawn at present.
Using 3Tesla MRI focal perivascular enhancement and oedema has been detected. The impact of inflammation on severity and prognosis of cerebral artery dissection is not known and is currently being investigated in the MRI-CAD study (Prof Simon Jung, Prof Marcel Arnold).