SWITCH: Decompressive Hemicraniectomy in Intracerebral Hemorrhage
The primary objective of this international randomized controlled trial is to determine whether decompressive surgery and best medical treatment in patients with spontaneous ICH will improve outcome compared to best medical treatment only
Introduction
Spontaneous intracerebral hemorrhage (ICH) remains a devastating disease with mortality rates up to 52% at 30 days. It is a major public health problem with an annual incidence of 10-30 per 100'000 population, accounting for 2 million (10-15%) of about 15 million strokes worldwide each year. The strategy of decompressive craniectomy (DC) is beneficial in patients with malignant middle cerebral artery (MCA) infarction. Based on the common pathophysiological mechanisms of these two conditions, this procedure is also frequently performed in patients with ICH, but has not yet been investigated in a randomized trial.
Why is ICH so devastating?
ICH is the most severe form of stroke. The hemorrhage damages the brain both directly, by destruction of brain tissue, and indirectly by increasing the pressure within the brain. Previous trials have investigated surgical removal of the hematoma. The results were disappointing and the two most recent, carefully performed and important trials (STICH and STICH II) failed to show a benefit after surgical removal of the hematoma. Surgical removal of the hematoma is thought to be ineffective due to additional trauma to the brain. Therefore new concepts are urgently needed to find treatment solutions for this devastating disease.
New concept
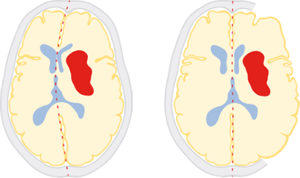
Decompressive craniectomy decreases intracranial pressure without further damage to the vulnerable brain. During this procedure the bone of the skull is removed, enabling the brain to expand and thereby reducing intracranial pressure. Decompressive craniectomy is a well-established treatment in patients with large ischemic strokes (major trials: DESTINY, HAMLET, DECIMAL).
Key inclusion- and exclusion criteria
Inclusion criteria
- Age: ≥18 to ≤75 years
- Acute stroke syndrome due to a spontaneous ICH
- Haemorrhage into basal ganglia, or thalamus that may extend into cerebral lobes, ventricles or subarachnoid space
- Glasgow coma scale (GCS) <14 and >7
- NIHSS ≥10 and ≤30
- Surgical treatment within 72 hours after ictus
- Volume of hematoma ≥30ml and ≤100ml
Exclusion criteria
- Intracranial aneurysm, brain arteriovenous malformation, brain tumor, brain trauma, stroke thrombolysis
- Cerebellar or brainstem hemorrhage
- Exclusive lobar hemorrhage
- Moribund patients (GCS 3-7)
Outcomes
Primary outcome measures
- Score in modified Rankin Scale (mRS) [ Time Frame: 6 months ]
- Assessed by telephone interview
Secondary outcome measures
- Mortality [ Time Frame: 7 days, 30 days, 180 days, 12 months ]
- mRS score of 0-3 versus 4-6 [ Time Frame: 30 days, 180 days, 12 months ]
- Categorical shift in mRS score [ Time Frame: 180 days, 12 months ]
- Quality of life [ Time Frame: 180 days, 12 months ]
- Death and intracranial hemorrhage [ Time Frame: intraoperative ]
Contact
Trial Core Team at SRCB

- Name / Titel
- Prof. Dr. med. Urs Fischer
- Funktion
- Consultant
- urs.fischer@insel.ch

- Name / Titel
- Prof. Dr. med. Werner Z'Graggen
- Funktion
- Consultant
- werner.zgraggen@insel.ch

- Name / Titel
- Prof. Dr. med. David Bervini
- Funktion
- Consultant
- david.bervini@insel.ch

- Name / Titel
- Dr. med. Johannes Goldberg
- Funktion
- Resident
- johannes.goldberg@insel.ch

- Name / Titel
- Dr. phil. Seraina Beyeler
- Funktion
- Clinical Trial Manager
- seraina.beyeler@insel.ch
- Phone
- +41 31 632 39 70
